
Enhancing Access to Care

Project Overview
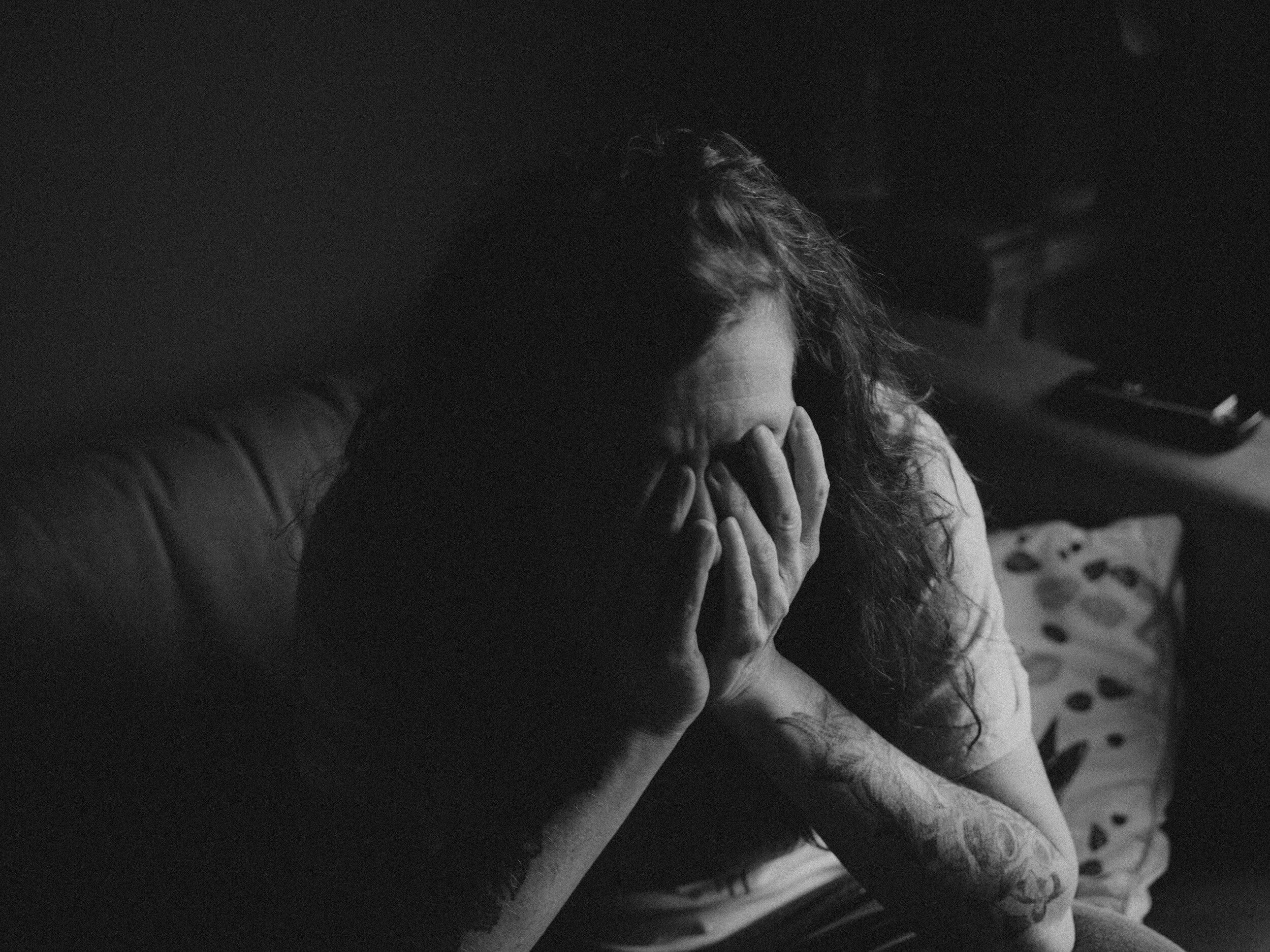
The goal of this UX research project is to identify new strategies to help improve access to behavioral health services for individuals in the state of Ohio. By employing user-centered design principles, we aim to identify barriers and pain points experienced by users seeking substance abuse and mental health support and develop user-centric solutions to address these challenges.

Research Objectives
Understand User Needs: Conduct in-depth interviews and surveys with individuals seeking behavioral health services, their families, and healthcare professionals to gain insights into their experiences, preferences, and pain points.
Identify Barriers: Explore the factors hindering access to behavioral health care, such as stigma, limited resources, geographical constraints, or lack of awareness about available services.
Investigate User Preferences: Explore user preferences concerning communication channels, appointment scheduling, virtual care options, and privacy concerns.
Address Inclusivity: Examine the accessibility of existing solutions to ensure they cater to individuals with diverse needs, including those with disabilities or language barriers.
Research Methodology
User Interviews: Conduct one-on-one interviews with individuals seeking behavioral health support, healthcare providers, counselors, and advocates. These interviews will provide qualitative insights into their experiences and perspectives.
Surveys: Distribute online surveys to gather quantitative data and reach a larger sample of users. The survey will cover topics related to user preferences, satisfaction levels, and challenges faced during their journey to access behavioral health services.
Comparative Analysis: Analyze existing resources available in Ohio to understand their strengths, weaknesses, and areas for improvement by comparing them to other states with similar population density.

Interview / Survey Questions
Can you describe the current state of behavioral health services in Ohio? Are there any specific challenges or gaps in access that you have observed?
What factors do you believe contribute to the lack of access to behavioral health treatment in the state? Are there any particular barriers that stand out?
In your opinion, how does the lack of integration between behavioral health services and primary healthcare settings hinder access to treatment for individuals in need?
Are there any notable disparities in access to behavioral health treatment between rural and urban areas in Ohio? If so, what are the contributing factors?
What role does insurance coverage play in determining an individual's access to behavioral health services? Are there any common challenges related to insurance coverage that you have observed?
Are there any specific populations in Ohio that face additional barriers to accessing behavioral health treatment? What strategies are in place to address the unique needs of these populations
Can you share any success stories or best practices from other regions or states that have effectively addressed the lack of access to behavioral health treatment? Are there any lessons that Ohio can learn from these examples?
How do community organizations and advocacy groups contribute to improving access to substance abuse and mental health treatment in Ohio? How can collaboration between these entities and government agencies be strengthened?
In your opinion, what are the most urgent priorities for addressing the lack of access to substance abuse and mental health treatment in Ohio? What are the potential long-term solutions?
How do you envision the ideal behavioral health treatment system in Ohio? What steps can be taken to work towards that vision?

Integration of Med and SUD /MH
Survey Results
Total surveys completed - 382
Potential Barriers
Most Affected Populations

Interview Quotes
(Questions were tailored depending on the person as we interviewed and surveyed service providers and community members as well as victims of substance abuse and behavioral health)
Prominent Private Practitioner - “My idea of an effective Ohio behavioral health system is one that is truly inclusive regarding all of the services that are possibly available to the people that need them most”
Active User - “ I just believe people should be able to get help when they actually need it, regardless of where they live”.
CEO of Non Profit substance abuse agency - “There are enough potential clients to go around, the competition from other agencies need to be put aside in order to create a community that is truly healthy.”
Jail administrator of a county in rural Ohio - “ I keep seeing the same faces in and out of this place, I would love to get people linked to treatment before they are released.
Prominent business owner - “My wife and I dealt with this, our son is addicted to crystal meth. We tried countless times to get him into a program but it always seemed to take so long. By the time he was able to be accepted he had simply lost interest.”
Founder and operator of a popular food pantry - “It just breaks my heart to see some of our community members actively addicted to drugs. Our county is considered rural and people simply do not have the resources to travel to the city for help.”

Comparative Analysis
Total Access
Fatal Overdose Rate

Key Insights and Opportunities
Increasing access to substance abuse and mental health services in the state of Ohio requires a multifaceted approach that involves collaboration between government agencies, healthcare providers, community organizations, and other stakeholders. Based upon the finding of the research conducted the following has been identified as potential initiatives to improve access in the state of Ohio:
Funding and resources: Allocate sufficient funds and resources to expand existing substance abuse treatment centers and establish new facilities in underserved areas. This can help increase the capacity to provide services and reduce waiting times for treatment.
Telehealth services: Implement and promote tele-health services for substance abuse treatment, especially in rural or remote areas where access to in-person services may be limited. Telehealth can provide counseling, therapy, and support remotely, making treatment more accessible.
Educational programs: Raise awareness about substance abuse issues and available resources through educational campaigns. This can help reduce stigma, encourage early intervention, and inform individuals about the benefits of seeking treatment.
Mobile treatment units: Utilize mobile treatment units to reach populations with limited access to traditional treatment centers. These units can bring healthcare professionals and resources to underserved communities.
Collaboration with primary care providers: Integrate substance abuse screening and treatment into primary healthcare settings to identify and address substance abuse issues at an early stage.
Criminal justice system reform: Implement diversion programs and treatment alternatives for non-violent drug offenders to provide them with access to rehabilitation instead of incarceration.
Specialized programs for vulnerable populations: Develop targeted substance abuse services for specific vulnerable populations, such as pregnant women, veterans, LGBTQ+ individuals, and the homeless.
24/7 helplines: Set up and promote helplines that offer information, support, and referrals to treatment options to assist those in crisis at any time.
Insurance coverage and reimbursement: Advocate for comprehensive insurance coverage of substance abuse treatment to reduce financial barriers for individuals seeking help.
Research and evaluation: Invest in research to identify effective strategies and continually evaluate programs' outcomes to optimize their impact.

